Remote Monitoring Helps Achieve Healthcare's Triple Aim
The healthcare industry is in the midst of a transition from ‘healthcare’ to ‘health optimization’ and remote monitoring technology will play a crucial role.
Enhancing care experience and outcomes, improving population health, and reducing costs is healthcare’s Triple Aim, a concept designed to shift focus from “healthcare” to “health optimization.” Several pilot programs, led by senior living providers and managed care organizations, suggest remote monitoring technology can play a crucial role in achieving these objectives.
 Today’s passive sensor technology monitors key wellness indicators – such as sleep quality, daily activities, and other physiological information – alerting caregivers to potential emergent health conditions. This results in more informed and proactive care decisions that reduce costs and slow the patient’s progression through the care continuum.
Today’s passive sensor technology monitors key wellness indicators – such as sleep quality, daily activities, and other physiological information – alerting caregivers to potential emergent health conditions. This results in more informed and proactive care decisions that reduce costs and slow the patient’s progression through the care continuum.
The goal should always be to prolong wellness, to keep individuals healthier, and allow them to age well in place. This takes on even greater urgency when one considers the current state of affairs. An acute shortage of both skilled nursing facilities and skilled nurses, rising acuity rates, and a higher cost of care are exacerbated by the fact that the number of Americans over 65 will more than double from 40 million in 2010 to 88 million by 2050, according to the U.S. Census Bureau.
There are three areas to consider when examining how remote monitoring impacts the Triple Aim: 1) improving health; 2) enhancing care; and 3) reducing costs.
Improving health
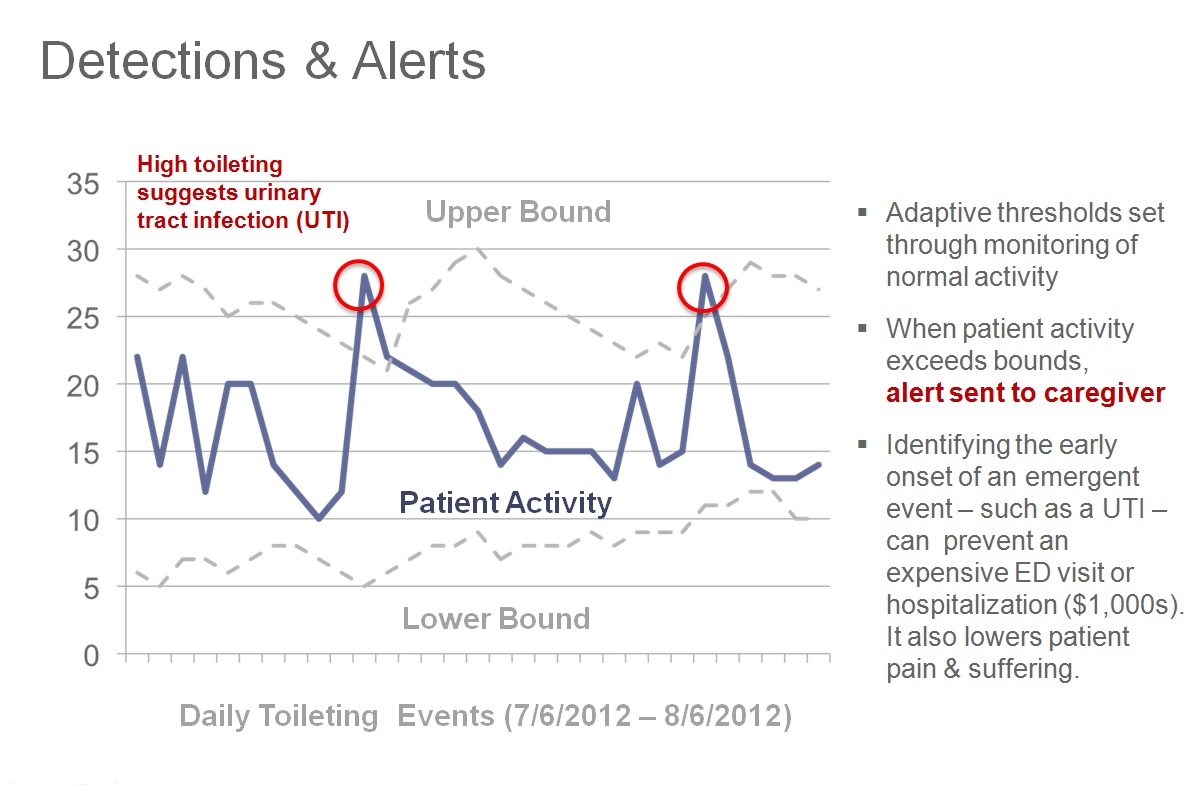
Remote monitoring provides 24/7 health and wellness oversight. For senior living communities specifically, sensors are utilized to track activities of daily living (ADLs) and determine the typical levels of daily activity for each resident.
This daily routine becomes the benchmark for establishing when assistance may be needed. In other words, rather than a request or other action by the resident such as pulling a cord or pushing a button, the intervention decision is based upon a significant change in an ADL pattern that may indicate exacerbation of a chronic condition or an acute illness. This information, delivered in real time or near-real time, allows for an immediate intervention before an individual’s condition deteriorates to the point where a visit to the emergency room or an inpatient stay is inevitable.
When managed care organizations and case managers are involved, remote monitoring provides them with information they wouldn’t otherwise be aware of due to infrequent home visits (some home visits take place just once a year for the patient’s annual health assessment).
Avoiding admissions and readmissions is a key metric upon which remote monitoring has had a measurable impact.
Enhancing care
Remote monitoring enhances care by identifying behavior patterns and changes in ADLs so that patients and caregivers can be alerted to potential problems at the earliest possible stage. This, in turn, allows people to remain independent for as long as possible while ensuring higher-acuity services are available to those who truly need them.
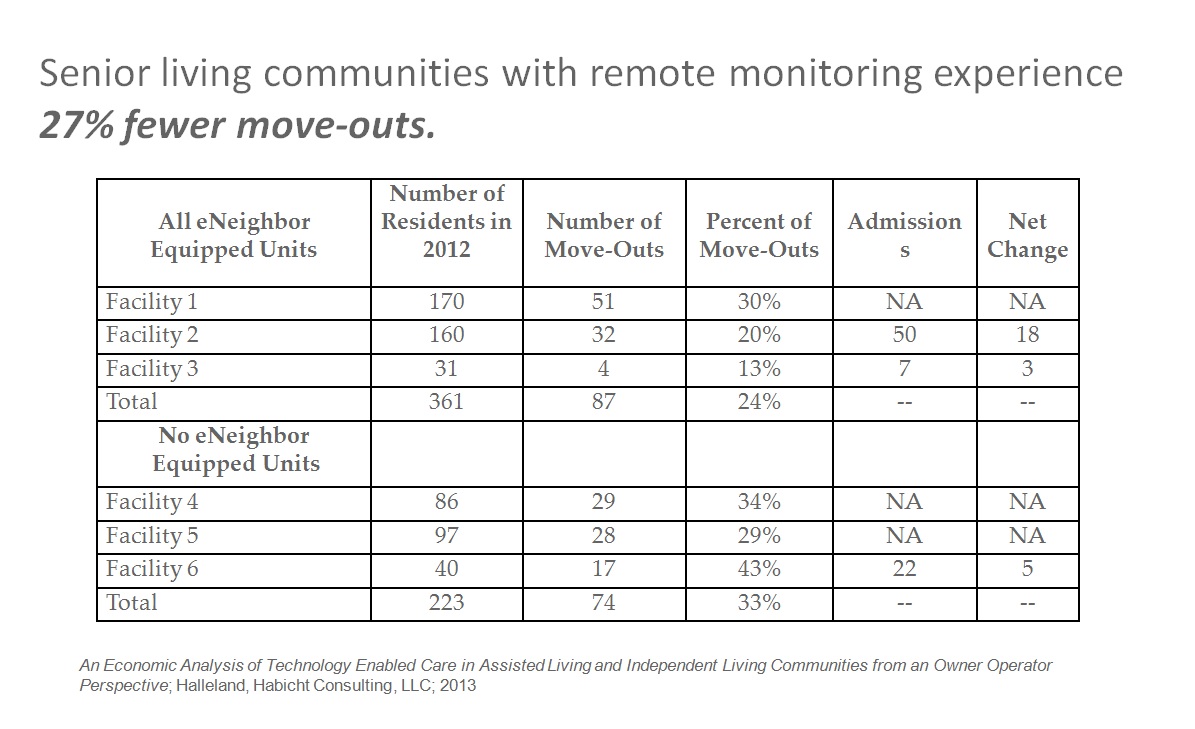 Supporting this is a recent economic analysis which found that assisted/independent living communities deploying remote monitoring technology with emergency response capabilities increase length-of-stay by reducing the number of discharges to higher-acuity care settings, and increase the services delivered in-place. The percentage of move-outs in these communities is 27 percent lower than those without.
Supporting this is a recent economic analysis which found that assisted/independent living communities deploying remote monitoring technology with emergency response capabilities increase length-of-stay by reducing the number of discharges to higher-acuity care settings, and increase the services delivered in-place. The percentage of move-outs in these communities is 27 percent lower than those without.
Consider the term “care pathway.” It describes the delivery of key care elements, based on Evidence-Based Medicine (EBM) guidelines, from the time an encounter begins in a doctor’s office, hospital or emergency room. The difficulty is, by that time, patients are often already very sick.
Remote monitoring, on the other hand, is a “pre-care pathway.” Care is enhanced and independent living prolonged by promoting health and wellness at an early stage, thus avoiding a more acute path.
Care is further enhanced because the 24/7 passive monitoring system requires nothing of the patient. It eases concerns of the patient’s loved ones while helping caregivers focus on the patient at the right time.
Reducing costs
Lastly, remote monitoring reduces costs by identifying health issues early, before they become more serious conditions requiring repeated ER and/or hospital visits. This also allows individuals to remain in their homes longer, further reducing costs by delaying or preventing more expensive care.
Remote monitoring places the focus on preventing problems through early interventions based on real-time sensor data, rather than reacting to acute situations after the fact. This appropriately complements the edicts of healthcare reform, which reward quality rather than quantity.
Essentially, reducing costs focuses on preventing avoidable ER visits and hospitalizations, including the prevention of readmission after an episode. Doing so consistently can reduce long-term care costs, which reached $357 billion in 2011, according to the Kaiser Family Foundation, and also help ease the growing shortage of higher-acuity care.
It’s all about the patients
The impact of remote monitoring on the Triple Aim, in particular its impact on improving care outcomes, is the focus of pilot programs underway by Humana Cares/Senior Bridge and Fallon Community Health Plan. Though it is too early for hard data, there is ample anecdotal evidence to suggest that the impact is positive.
For example, in the case of Margaret, remote sensor data indicated that she was up frequently at night. When she managed to sleep, it was usually restlessly, indicated by frequent bed monitor “loading” and “unloading.” Combine this with a decrease in toileting and eating patterns over a week’s time, and it is clear that there was cause for concern.
 Another piece of the puzzle was contained in Margaret’s medical record, where her case manager had documented that she was experiencing flu-like symptoms. Her caregiver was alerted and an appointment was made for Margaret to see her doctor, who ultimately diagnosed an exacerbation of COPD, resulting in a prescribed steroid medication.
Another piece of the puzzle was contained in Margaret’s medical record, where her case manager had documented that she was experiencing flu-like symptoms. Her caregiver was alerted and an appointment was made for Margaret to see her doctor, who ultimately diagnosed an exacerbation of COPD, resulting in a prescribed steroid medication.
Without remote monitoring, it is likely Margaret would have been taken to the ER for shortness of breath. For COPD patients in particular, such visits typically lead to hospital admission. But by alerting her caregiver to the change in ADLs, this visit was avoided altogether.
In another example, sensors in 86-year-old Nancy’s home detected an increase bed loading and unloading and in movement throughout her apartment. Her care manager was alerted to the changes in patterns. An evaluation revealed that Nancy was having trouble keeping track of medical appointments, was suffering from increased depression due to a recent dementia diagnosis and was having difficulties with her balance, putting her at risk for falls. Nancy also told her care manager that she was sending thousands of dollars to scam mailings.
Based on these findings, the care manager changed Nancy’s care plan to increase day programming and homemaking services, and added treatment for her depression. As a result, Nancy is sleeping better at night, which reduces her susceptibility to a fall, which the Centers for Disease Control and Prevention estimates costs an average of $17,132.
Nancy’s family is investigating financial fraud and is focusing more on managing her finances, to preserve her financial security. Her son is also now acting as Nancy’s main healthcare agent, taking a more active role in her Advanced Directives/Physician Orders for Life-Sustaining Treatment (POLST).
The Triple Aim and beyond
The goal of remote monitoring isn’t to steer caregivers toward a specific diagnosis. Rather, it is to alert care teams and providers to underlying symptoms that point to the larger picture to make a clinical judgment.
Remote monitoring technology can play a crucial role in achieving the objectives of the Triple Aim by alerting caregivers to potential emergent health conditions. This leads to more informed and proactive care decisions that reduce costs and slow the patient’s progression through the care continuum.
About the author
Julie Carr, RN, BSN, is Nursing and Clinical Services Manager of Healthsense, Inc. and can be reached at Julie.Carr@Healthsense.com.
